Macular Pucker
The macula is the small area at the center of the eye’s retina that allows you to see fine details clearly. The retina is a layer of light-sensing cells lining the back of your eye.
As light rays enter your eye, the retina converts the rays into signals, which are sent through the optic nerve to your brain where they are recognized as images.
Damage to your macula causes blurred central vision, making it difficult to perform tasks such as reading small print or threading a needle.
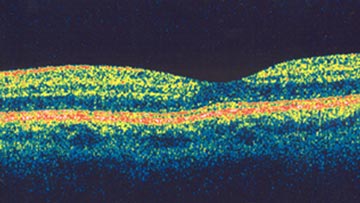
OCT cross-sectional image of a normal fovea, the center of the macula.
What is a macular pucker?
The macula normally lies flat against the back of the eye, like film lining the back of a camera. When wrinkles, creases or bulges form on the macula, this is known as macular pucker. It is typically caused by a thin membrane growing on the macula, an epiretinal membrane.
Ophthalmologists use tiny instruments to remove the wrinkled tissue on the macula.
What are the symptoms of macular pucker?
Symptoms of macular pucker range from mild to severe and may involve one or both eyes. Symptoms may include:
- Blurred central (detail) vision
- Distorted, or wavy, vision
- Difficulty reading or performing tasks that require detail vision
- Gray and/or cloudy area in central vision
- Central blind spot
- Peripheral (side) vision is not affected.
What causes macular pucker?
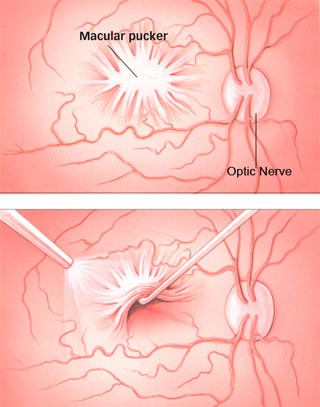
Ophthalmologists use tiny instruments to remove the wrinkled tissue on the macula.
As you age, the vitreous humour, the clear, gel-like substance that fills the middle of your eye begins to shrink and pull away from the retina. As the vitreous pulls away, scar tissue may develop on the macula. Sometimes the scar tissue can warp and contract, causing the retina to wrinkle or bulge.
Eye conditions associated with macular pucker include:
- vitreous detachment
- torn or detached retina
- inflammation inside the eye
- severe trauma to the eye (from surgery or injury)
- disorders of the blood vessels in the retina
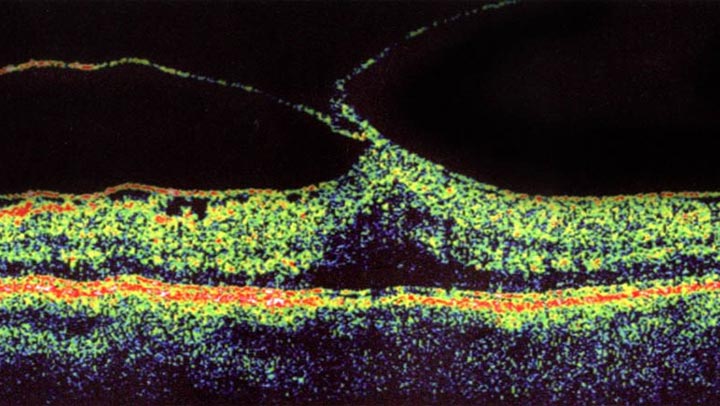
Epiretinal membrane seen pulling the macula up causing decreased and distorted vision.
How is macular pucker detected?
Your ophthalmologist (Eye M.D.) detects macular pucker by examining your retina. Your doctor may perform fluorescein angiography or optical coherence tomography (OCT) procedures that take special photographs of the eye. These photographs show if an abnormality exists in your retina.
How is macular pucker treated?
For mild symptoms, no treatment may be necessary. Updating your eyeglass prescription or wearing bifocals may improve vision. Eyedrops, medicines or laser surgery do not improve vision.
For more severe symptoms, a surgery called vitrectomy is recommended. The surgery is usually performed as an outpatient procedure in an operating room. During surgery, your ophthalmologist uses tiny instruments to remove the wrinkled tissue on your macula. After the tissue is gone, the macula flattens and vision slowly improves, though it usually does not return all the way to normal. You should consider surgery if your blurred vision is interfering with your daily activities.
Are there any risks involved with vitrectomy surgery?
As with any surgical procedure, complications can occur with vitrectomy surgery. Complications may include:
- Infection
- Bleeding
- Retinal detachment
- Recurrence of macular pucker
After vitrectomy surgery, cataracts (clouding of the eye’s lens) may also develop. Be sure to discuss potential complications with your ophthalmologist before surgery.
Macular Pucker
Macular Pucker Vitrectomy
Article Videos
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.