Cataract
What is a cataract?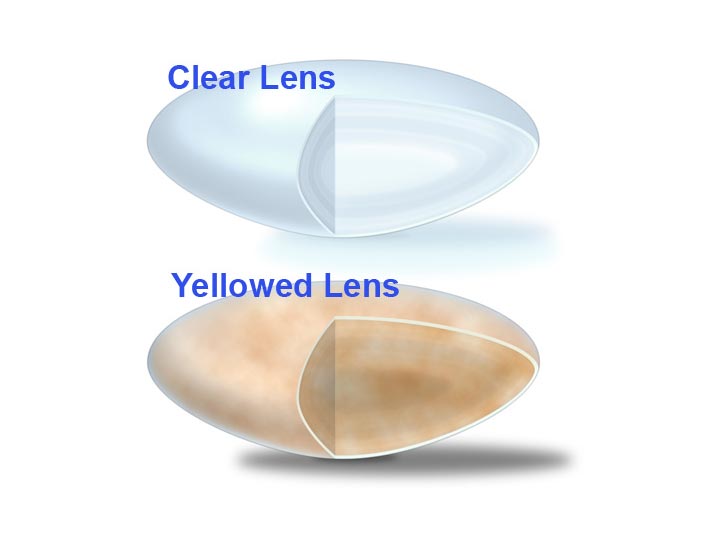
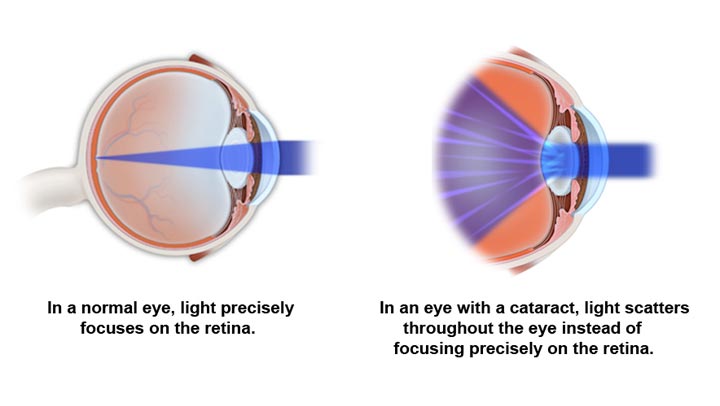
A cataract is a clouding of the normally clear lens of the eye. It can be compared to a window that is frosted or yellowed.
The amount and pattern of the cloudiness within the lens can vary. If the cloudiness is not near the center of the lens, you may not be aware that a cataract is present.
A cataract is not:
- A film over the eye
- Caused by overusing the eyes
- Spread from one eye to the other
- A cause of irreversible blindness
Common symptoms of cataract include:
- A painless blurring of vision
- Glare, or light sensitivity
- Poor night vision
- Double vision in one eye
- Needing brighter light to read
- Fading or yellowing of colors
What causes cataract?

The most common type of cataract is related to aging of the eye.
Causes of cataract include:
- Family history
- Medical problems, such as diabetes
- Injury to the eye
- Medications, especially steroids
- Radiation
- Long-term, unprotected exposure to sunlight
- Pprevious eye surgery
- Unknown factors
How fast does a cataract develop?
How quickly a cataract develops varies among individuals and may even be different between the two eyes. Most age-related cataracts progress gradually over a period of years. Other cataracts, especially in younger people and people with diabetes, may progress rapidly over a short time. It is not possible to predict exactly how fast cataracts will develop in any given person.
How is cataract treated?
Surgery is the only way a cataract can be removed. However, if symptoms of cataract are not bothering you, surgery may not be needed. Sometimes a simple change in your eyeglass prescription may be helpful.
No medications, dietary supplements or exercises have been shown to prevent or cure cataracts. Protection from excessive sunlight may help slow the progression of cataracts. Sunglasses that screen out ultraviolet (UV) light rays or regular eyeglasses with a clear, anti-UV coating offer this protection.
How is a cataract detected?
By performing a thorough eye examination, your ophthalmologist (Eye M.D.) can detect the presence of a cataract. A careful evaluation will also rule out any other conditions that may be causing blurred vision or other eye problems. Problems with other parts of the eye (such as cornea, retina or optic nerve) can be responsible for vision loss and may prevent you from having much or any improvement in vision after cataract surgery. If improvement in your vision is unlikely, cataract removal may not be recommended. Your ophthalmologist can tell you how much visual improvement is likely.
When should surgery be done?
Surgery should be considered when cataracts cause enough loss of vision to interfere with your daily activities. It is not true that cataracts need to be “ripe” before they can be removed or that they need to be removed just because they are present.
Cataract surgery can be performed when your visual needs require it. You must decide if you can see well enough to do your job, drive safely, and read or watch TV in comfort. Does your vision allow you to perform daily tasks such as cooking, shopping, doing yard work or taking medications without difficulty?
Based on your symptoms, you and your ophthalmologist should decide together when surgery is appropriate.
What can I expect from cataract surgery?
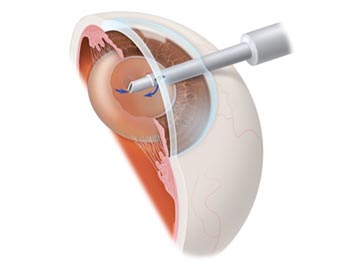
Over 1.4 million people have cataract surgery each year in the United States, and more than 95% of those surgeries are performed with no complications. During cataract surgery, which is usually performed under local or topical anesthesia as an outpatient procedure, the cloudy lens is removed from the eye.
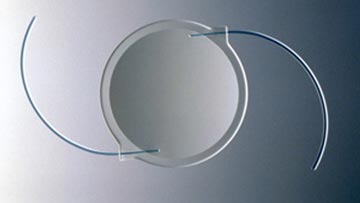
In most cases, the focusing power of the natural lens is restored by replacing it with a permanent intraocular lens implant. Read more about Intraocular Lenses.
Your ophthalmologist performs this delicate surgery using a microscope, miniature instruments and other modern technology. After surgery, you will have to take eye drops as your ophthalmologist directs. Your surgeon will check your eye several times after surgery to make sure it is healing properly.
Cataract surgery is a highly successful procedure. Improved vision is the result in over 95% of cases, unless there is a problem with the cornea, retina, optic nerve or other structures. It is important to understand that complications can occur during or after the surgery, some severe enough to limit vision. If you experience even the slightest problem after cataract surgery, your ophthalmologist will want to hear from you immediately.
For many people after cataract surgery, a film develops on the natural capsule that supports the lens implant causing vision to become cloudy. If this occurs, your ophthalmologist can perform an outpatient laser procedure to open this cloudy capsule, restoring clear vision. Read more about Posterior Laser Capsulotomy.

Conclusion
Cataracts are a common cause of decreased vision, particularly for the elderly, but they are treatable.
Your ophthalmologist can tell you whether cataract or some other problem is the cause of your vision loss and can help you decide if cataract surgery is appropriate for you.
How The Eye Sees As a Cataract Forms
Cataract Formation
Cataract Surgery
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.