Fuchs’ Corneal Dystrophy
Fuchs’ dystrophy is a progressive disease affecting the part of the eye called the cornea.
The cornea is like the crystal covering a clock face. It is a clear, round dome covering the iris, the colored ring in the center of the eye, and the pupil, the black circle in the middle of the iris. By helping to focus light as it enters the eye, the cornea plays an important role in vision.
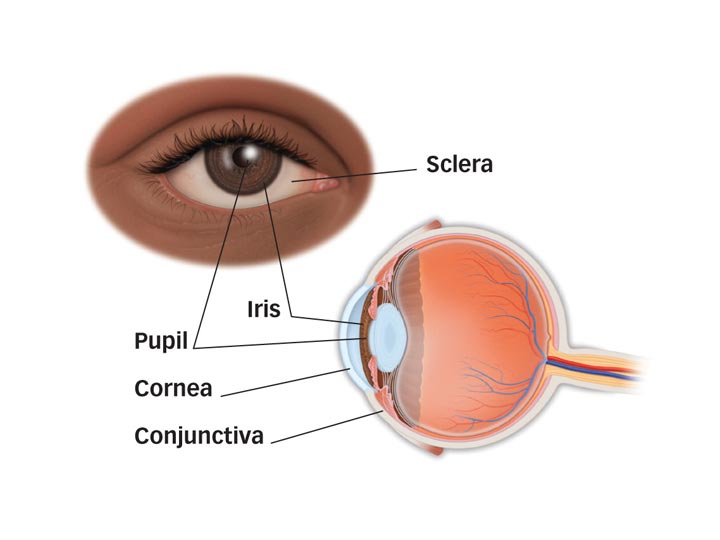
Front and side views showing parts of the eye. The cornea is the eye’s clear, dome-shaped covering.
Fuchs’ dystrophy reduces the number of specific cells (called endothelial cells) that make up the inner layer of the cornea. This reduction of cells causes the cornea to become unusually thick or puffy. Also seen in Fuchs’ dystrophy are dewdrop-shaped outgrowths called guttata in the layer just underneath the endothelial cell layer called Descemet’s membrane.
These cell changes may cause the cornea to become swollen and cloudy, losing its crystal-clear transparency. Because Fuchs’ dystrophy is a progressive disease, over time, changes to the corneal cells may interfere with vision.
Fuchs’ dystrophy usually occurs after age 40. Studies show that it is an inherited condition.
What are the symptoms of Fuchs’ dystrophy?
A person with Fuchs’ dystrophy may have hazy or cloudy vision, with the disease usually developing over two stages.
Stage 1 may produce no symptoms or only mild symptoms. In this early stage, the swelling of the corneal cells usually occurs in the morning then tends to clear as the day progresses. Vision is worse in the morning because closing your eyes during sleep keeps moisture from evaporating out of the cornea.
Once the disease has progressed to Stage 2, vision no longer gets better later in the day. People with Stage 2 Fuchs’ dystrophy may have pain and sensitivity to light. Extreme climate conditions, such as high humidity, can worsen the condition.
Over time, some people with Stage 2 Fuchs’ dystrophy develop scarring at the center of their cornea. Once scarring is present, the patient may become more comfortable, but the film of scar tissue over the cornea reduces vision.
It can take 10 to 20 years or longer for Fuchs’ dystrophy to progress from its early to late stage. If the end stage of Fuchs’ dystrophy results in significant vision loss, your ophthalmologist (Eye M.D.) can perform corneal transplant surgery. Fortunately, in the majority of patients, Fuchs’ dystrophy does not progress so far that corneal transplant surgery is needed.
How is Fuchs’ dystrophy diagnosed?
To diagnose Fuchs’ dystrophy, your ophthalmologist checks for guttata with an instrument called a slit-lamp biomicroscope. Your ophthalmologist may also measure the thickness of the cornea or take a special photograph of the endothelial cell layer to get an actual cell count. These examinations are brief and do not cause any pain.
How is Fuchs’ dystrophy treated?
Treatment for Fuchs’ dystrophy depends on your particular condition, such as whether you have a cataract and the degree of changes in your corneal cells.
To control Stage 1 of the disease, your ophthalmologist may prescribe one or more of the following treatments:
- Applying eyedrops to lessen swelling of the cells in the cornea
- Using a hair dryer, held at arm’s length, to help dry the surface of the cornea
- In Stage 2, you may need to wear a therapeutic bandage contact lens to lessen discomfort
If poor vision begins to affect your lifestyle, your ophthalmologist may recommend corneal transplant surgery. There are two transplant options available: endothelial keratoplasty, a new method that transplants the endothelium and inner layers of the cornea, and penetrating keratoplasty, a transplant of the entire central part of the cornea. Both procedures are effective, though endothelial keratoplasty is becoming more popular due to its shorter recovery time.
Some patients who have additional eye problems, such as cataracts, will need more complex surgeries that involve additional procedures. Your ophthalmologist will explain the treatment options appropriate for your case and will be happy to answer any questions you might have.
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.