Microvascular Cranial Nerve Palsy
Microvascular Cranial Nerve Palsy (MCNP) is one of the most common causes of acute double vision in the older population.
It occurs more often in patients with diabetes and high blood pressure. MCNP is sometimes referred to as a “diabetic” palsy. This condition almost always resolves on its own without leaving any double vision.
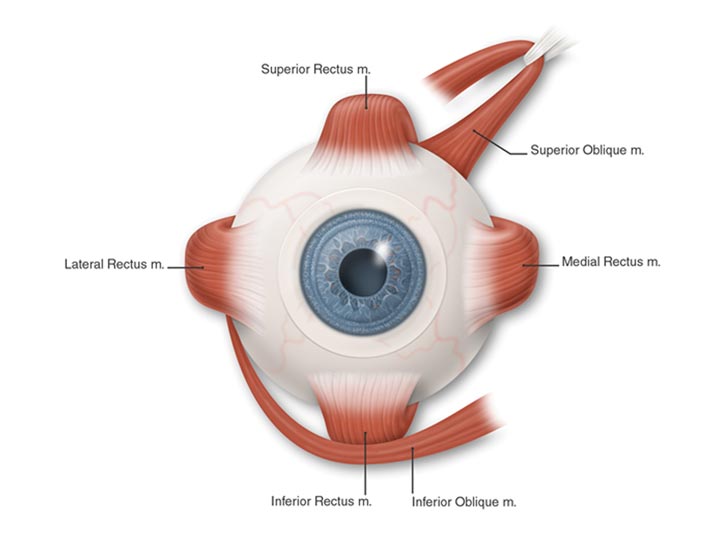
Eye Muscles (Anterior)
Six muscles move your eyes. Four of these muscles attach to the front part of your eye (just behind the iris, or the colored portion of the eye). Two muscles that attach to the back of your eye are responsible for some of the up-and-down (vertical) movement and most of the twisting movement of each eye. These six muscles receive their signals from three cranial nerves that begin in the brain stem.
What is Microvascular Cranial Nerve Palsy?
A nerve cannot function properly when its blood flow is blocked. If the 6th cranial nerve (also called the abducens nerve) is affected, your eye will not be able to move to the outside and you will be aware of double vision, seeing side-by-side images. If the 4th cranial nerve (also called the trochlear nerve) is affected, you will be aware of vertical double vision (one image on top of another). You may be able to eliminate or decrease the double vision by tilting your head towards the opposite shoulder.
The 3rd cranial nerve (also called the oculomotor nerve) supplies four of the six eye muscles. These are some of the muscles that control the eyelid and the size of the pupil. When the 3rd cranial nerve is affected, your eye may be limited in its up-and-down motion and may turn away from your nose. The eyelid may droop. You usually experience combined vertical and side-by-side double vision.
What causes microvascular cranial nerve palsy?
It is not always clear what causes the blockage in the tiny blood vessels to the cranial nerves. In some cases, diabetes or high blood pressure may be risk factors. In young patients, migraine may affect these tiny vessels. Occasionally there may also be a blocked vessel in the covering of the brain, which can be associated with pain around the eye. The nerves are not permanently injured, and over a period of six to 12 weeks, normal function should recover. If the double vision does not go away, it is very important to tell your ophthalmologist (Eye M.D.).
What are the signs and symptoms of microvascular cranial nerve palsy?
The signs of MCNP are usually problems with movement of your eyes that lead to blurred or double vision. If severely affected, your eye may not be able to move at all in one or more directions. Sometimes there may only be a slowing of movement.
Symptoms may include:
- Weakness in one or more eye muscles
- Blurred vision that improves by closing either eye
- Double vision
- Pain in or around the eye (related to lack of blood flow to the covering of the brain), which commonly occurs at the onset of double vision
- Drooping eyelid (called ptosis)
- Enlarged pupil (rarely)
A careful description of these symptoms is important to your ophthalmologist. He or she will perform a complete medical eye examination to help determine what pattern your double vision fits and whether or not it is an isolated cranial nerve weakness. If you have multiple microvascular cranial nerve palsies, involvement of the pupil, or have onset at a younger age, a neurologic exam and imaging study (such as CT, MRI scan, or angiogram) may be necessary. Anyone diagnosed with MCNP should have their blood pressure and blood sugar checked to make sure they do not have diabetes or hypertension.
How is microvascular cranial nerve palsy treated?
There is no way to speed the natural recovery time for MCNP. Double vision may be treated by patching either eye. If the double vision persists, it may be possible to use prism glasses or to consider eye muscle surgery if recovery has not been complete. Anti-inflammatory drugs such as ibuprofen (Advil? or Motrin?) may help if there is associated pain with MCNP. It is important to make sure that blood pressure and blood sugar are adequately controlled.
It is very important to tell your doctor if you have new symptoms of double vision or if your double vision fails to resolve. Risk factors that increase the chance of microvascular cranial nerve palsy (such as diabetes, high blood pressure, and smoking) also increase your risk of stroke. It is important that your doctor check to make sure that any risk factors you have be reduced or treated.
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.