Refractive Surgery & Laser Vision Correction
Refractive surgery improves vision by permanently changing the shape of the cornea, the clear front window of the eye.
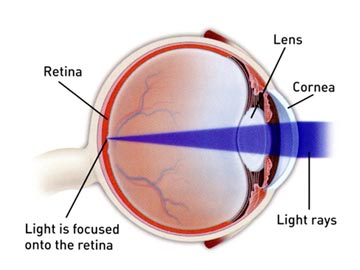 When treating myopia or nearsightedness, refractive surgery techniques reduce the curvature of the cornea to lessen the eye’s focusing power. Images that are focused in front of the retina, due to an elongated eye or steep corneal curve, are pushed closer to or directly onto the retina.
When treating myopia or nearsightedness, refractive surgery techniques reduce the curvature of the cornea to lessen the eye’s focusing power. Images that are focused in front of the retina, due to an elongated eye or steep corneal curve, are pushed closer to or directly onto the retina.
When treating hyperopia or farsightedness, refractive surgery techniques make the cornea steeper to increase the eye’s focusing power. Images that are focused beyond the retina, due to a short eye or thin cornea, are pulled closer to or directly onto the retina.
Astigmatism occurs when the cornea is more curved in one direction than the other. If astigmatism is significant, light passing through the cornea is scattered. Images reaching the retina are distorted and vision is blurred. When treating astigmatism, refractive surgery techniques selectively reshape portions of the cornea to make it symmetrical and smooth, so that images focus clearly on the retina.
Common refractive surgery procedures include:
- Photorefractive keratectomy (PRK)
- Laser in situ keratomileusis (LASIK)
- Astigmatic keratotomy (AK)
- Intrastromal corneal rings
Photorefractive keratectomy (PRK)
PRK is a surgical procedure in which the surgeon uses a laser to remove micro-thin layers of tissue from the cornea. The tissue is removed in a controlled pattern programmed into the computer by the surgeon.
When treating myopia, or nearsightedness, the surgeon uses the laser to flatten the corneal surface in a circular pattern. In comparison, when treating astigmatism, the laser is programmed to remove tissue in an elliptical pattern, selectively reshaping some portions of the cornea to form a smooth symmetrical surface. This procedure requires precise evaluation of the astigmatism so that the correct amounts of laser energy are delivered to the appropriate areas of the cornea.
Laser in situ keratomileusis (LASIK):
LASIK is a combined microsurgical and excimer laser procedure used to correct myopia, hyperopia and astigmatism. In LASIK, a highly specialized instrument, the microkeratome, is used to make a thin flap in the cornea. The excimer laser is applied beneath the corneal flap. The flap is then replaced and allowed to heal. No stitches are necessary. Femtosecond lasers can also be used to create the flap.
Wavefront-Guided LASIK
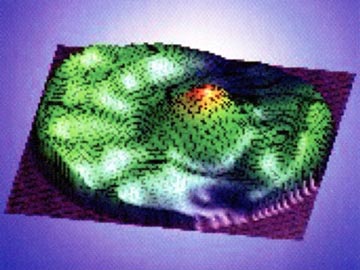
Wavefront Map
An enhanced version of LASIK called wavefront-guided custom laser surgery, or wavefront-guided LASIK, uses a special device to precisely measure the eye’s unique irregularities and variations.
If wavefront-guided LASIK is an option for you, you may benefit from this customized approach to refractive surgery, which results in improved quality of vision compared to the traditional approach.
To understand how wavefront works, it’s important to understand how your eye focuses light.
A perfect cornea allows light entering the eye to be focused evenly through the pupil and then fine-tuned by the eye’s natural lens so that light rays fall precisely onto the retina.
Small imperfections in the eye cause some light to travel through the eye at different angles. It is these imperfections that can cause the light to strike the retina in different places. As a result, you may experience symptoms like halos, glare, starbursts, or ghosting of images.
The wavefront map is very detailed: it is similar to a topographical map that records every subtle curve and dip. In fact, you might hear wavefront described as a fingerprint of your eye, because it measures tiny, subtle variations in the eye that are as unique as your fingerprints.
Measuring your eye with wavefront technology before performing LASIK can help your ophthalmologist enhance the outcome of surgery, resulting in fewer visual side effects and improved quality of vision using the custom procedure, rather than a conventional approach.
Astigmatic keratotomy (AK)
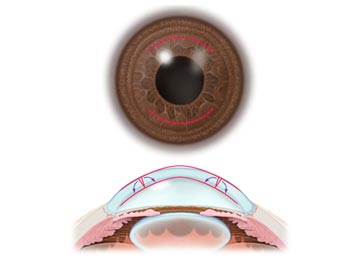 This procedure is generally used in combination with the excimer laser procedures when there is a need to correct both myopia and astigmatism, or as a “touch up” procedure if astigmatism remains after a prior laser procedure.
This procedure is generally used in combination with the excimer laser procedures when there is a need to correct both myopia and astigmatism, or as a “touch up” procedure if astigmatism remains after a prior laser procedure.
Astigmatic keratotomy is a microsurgical procedure in which the surgeon makes deep curved incisions in the cornea (usually one or two) to flatten the areas of the cornea that are too steeply curved.
As with any type of surgery, each refractive surgery technique has some potential complications and side effects. They include:
- fluctuating and blurry vision
- light sensitivity and glare
- under – or over-correction
- haze (except LASIK)
- haloes
- temporary discomfort
- reading glasses needed at an earlier age
Rare complications include
- cataract
- persistent pain
- serious infection
- permanent vision loss
Intrastromal corneal rings
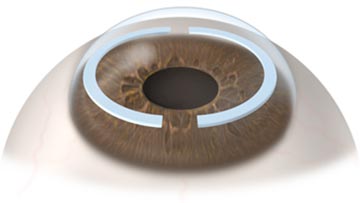

Intrastromal corneal rings, sometimes called intracorneal rings, are crescent-shaped plastic segments surgically implanted in the eye to flatten the cornea. They are used to correct mild nearsightedness.
Side effects include glare, haloes and problems with night vision. For most people,, these side effects are temporary, but for some, they do not go away. Intrastromal corneal rings can be removed. In some cases, vision returns to how it was before surgery, but some people may be left with permanent visual symptoms.
Surgical complications can lead to induced astigmatism, glare and haloes. Rare complications include infection, loss of best corrected vision, and penetration of the eye.
Which method is best?
There is no best method for correcting refractive errors. Discuss your needs and lifestyle with your ophthalmologist (Eye M.D.) to determine the best procedure for you.
Are you a good candidate for refractive surgery?
You might consider refractive surgery if you:
- Wish to decrease your dependence on glasses or contact lenses
- Are free of eye disease
- Can accept inherent risks and potential side effects of the procedure
- Have appropriate refractive error
While refractive surgery does offer some people an alternative to dependence on glasses or contact lenses, it’s not for everyone. You may not be a good candidate for refractive surgery if you are generally satisfied with glasses or contact lenses and unwilling to accept the uncertainty in the outcome of refractive procedures. Even after the refractive surgery, certain people may still need to wear glasses or contacts.
Surgery, contacts and glasses each have their benefits and drawbacks. The best method of correcting your vision should be decided after a thorough examination and discussion with your ophthalmologist.
Important facts
Ninety-five percent of people who have had refractive surgery can pass a standard driver’s license exam that requires a visual acuity of at least 20/40 without glasses or contacts.
Additional enhancement surgeries may be required to achieve your desired results.
You may still need glasses or contact lenses to achieve your best vision even after refractive surgery.
Fitting contact lenses may be difficult or impossible because of corneal changes following refractive surgery.
Reading glasses may still be necessary for middle-aged and older adults. Refractive surgery does not alter the aging process of the eye and does not prevent presbyopia. In fact, you may need reading glasses at a younger age.
If you have specific occupational goals, check with your prospective employer about regulations concerning refractive surgery.
PRK
Monovision
LASIK Microkeratome
LASIK Femto
LASEK
LASIK Wavefront
Astigmatic Keratotomy
Intrastromal Corneal Rings
RLE Phaco
RLE Femto
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.