Selective Laser Trabeculoplasty (SLT) for Glaucoma
What is Glaucoma?
Glaucoma is a disease of the optic nerve – the part of the eye that carries the images we see to the brain. The optic never is made up of many nerve fibers, like an electric cable containing numerous wires. When damage to the optic nerve fibers occurs, blind spots develop in our vision. These blind spots usually go unnoticed until the optic nerve is significantly damaged. If the entire optic nerve is destroyed, blindness results.
The most common form of glaucoma is chronic open angle glaucoma. In this condition, a part of the eye called the drainage channel becomes less efficient at draining microscopic amounts of fluid from the eye over time, allowing pressure within the eye to gradually increase. The increased pressure slowly and painlessly destroys the nerve fibers in the optic nerve.
Eyes have different abilities to withstand eye pressure. Some people can even develop glaucoma damage at normal pressures. When someone is at high risk for further nerve damage, treatment to lower eye pressure is necessary to prevent further vision loss. Early detection and treatment by your ophthalmologist (Eye M.D.) are the keys to preventing blindness from glaucoma.
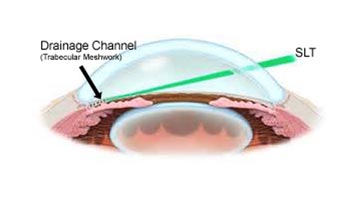
How can Selective Laser Trabeculoplasty (SLT) help treat open angle glaucoma?
Selective Laser Trabeculoplasty (SLT) uses a neodymium:YAG laser to focus light energy on the internal drainage channel of the ye. SLT targets the pigmented (melanin-containing) cells in the trabecular meshwork using a very short application of light. Because SLT uses a low amount of energy, the surrounding tissue is not damaged. The treatment allows the drain to work more efficiently, successfully lowering pressure more than 80 percent of the time.
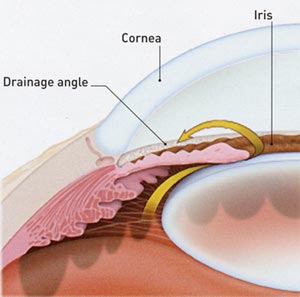
If the drainage angle is blocked, excess fluid cannot flow out of the eye, causing the fluid pressure to increase.
After SLT, your eye pressure may increase over time. By five years, up to half of people treated with SLT experience a rise in eye pressure. Your doctor will need to continue to monitor your eye pressure and can repeat the SLT treatment if needed, although retreatment may not be as successful as the initial treatment.
Who is a candidate for SLT?
Laser surgery can reduce the amount of medication you may need and is often recommended when you have trouble inserting eyedrops or are not using eyedrops on a regular basis. SLT can also be used in addition to medicines or as a first line of treatment.
What are the Risks of SLT?
As with any surgery, there are some risks of complications with SLT. Possible complications include:
- Failure to adequately lower the eye pressure
- Increased pressure in the eye, possibly requiring medications or surgery or both to lower it
- Inflammation in the eye causing pain, redness and or blurred vision
There are always risks associated with medications and surgery. However, the risks should be balanced against the greater risk of leaving glaucoma untreated and losing your vision.
If you have any questions about for glaucoma, you should discuss them with your Eye M.D.
How is SLT done?
The procedure is done in the ophthalmologist’s office or a laser treatment center and usually takes less than 10 minutes. First, anesthetic eye drops are used to numb the eye. Additional drops are given to control eye pressure, pupil size and inflammation.
While you are seated at the examining microscope, the laser energy is then focused through a lens to treat the drainage channel (trabecular meshwork). You will experience a flash of light with each laser application. There is rarely discomfort with this treatment.
After treatment your eye pressure will be monitored approximately one to two hours after the procedure. Very rarely, eye pressure can rise, requiring additional treatment. Anti-inflammatory eyedrops are often prescribed for several days after the procedure.
Your vision may be blurry immediately after treatment but should clear within hours, sometimes overnight. Most people can return to their normal activities the day after surgery.
It will take several weeks for the laser treatment to take full effect. Your doctor will want to check your eye pressure one to two months after the procedure. If you eye pressure is not lower at the first visit, some additional effect can be gained up to three months after treatment. If lower eye pressure is needed, your Eye M.D. will help you decide whether additional laser treatment, medication or other surgery is required.
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.