Glaucoma: What is it and how is it detected?
What is glaucoma?
Glaucoma is a disease of the optic nerve – the part of the eye that carries the images we see to the brain. The optic nerve is made up of many nerve fibers, like an electric cable containing numerous wires. When damage to the optic nerve fibers occurs, blind spots develop. These blind spots usually go undetected until the optic nerve is significantly damaged. If the entire nerve is destroyed, blindness results.
Early detection and treatment by your ophthalmologist (Eye M.D.) are the keys to preventing optic nerve damage and blindness from glaucoma. Glaucoma is a leading cause of blindness in the United States, especially for older people. but loss of sight from glaucoma can often be prevented with early treatment.
What causes glaucoma?
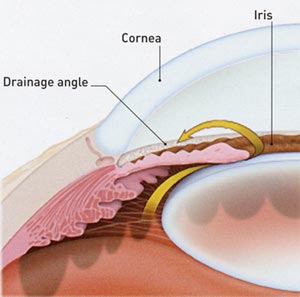
If the drainage angle is blocked, excess fluid cannot flow out of the eye, causing the fluid pressure to increase.
Clear liquid called aqueous humor circulates inside the front portion of the eye. To maintain a healthy level of pressure within the eye, a small amount of this fluid is produced constantly while an equal amount flows out of the eye through a microscopic drainage system. (This liquid is not part of the tears on the outer surface of the eye.)
If the drainage angle is blocked, excess fluid cannot flow out of the eye, causing the fluid pressure to increase.
Because the eye is a closed structure, if the drainage area for the aqueous humor-called the drainage angle-is blocked, the excess fluid cannot flow out of the eye. Fluid pressure within the eye increases, pushing against the optic nerve and causing damage. See this short video on Retinal Nerve Fibers and Glaucoma.
What are the different types of glaucoma?
Chronic -open-angle glaucoma: This is the most common form of glaucoma in the United States. The risk of developing chronic open-angle glaucoma increases with age. The drainage angle of the eye becomes less efficient over time, and pressure within the eye gradually increases, which can damage the optic nerve. In some patients, the optic nerve becomes sensitive even to normal eye pressure and is at risk for damage. Treatment is necessary to prevent further vision loss. See a short video on Open Angle Glaucoma.
Typically, open-angle glaucoma has no symptoms in its early stages, and vision remains normal. As the optic nerve becomes more damaged, blank spots begin to appear in your field of vision. You typically won’t notice these blank spots in your day-to-day activities until the optic nerve is significantly damaged and these spots become large. If all the optic nerve fibers die, blindness results. Follow this link to a short video on Glaucoma and Blind Spots.
Closed-angle glaucoma: Some eyes are formed with the iris (the colored part of the eye) too close to the drainage angle. In these eyes, which are often small and farsighted, the iris can be sucked into the drainage angle and block it completely. Since the fluid cannot exit the eye, pressure inside the eye builds rapidly and causes an acute closed-angle attack. Symptoms may include:
- blurred vision
- severe eye pain
- headache
- rainbow-colored halos around lights
- nausea and vomiting
This is a true eye emergency. If you have any of these symptoms, call your ophthalmologist immediately. Unless this type of glaucoma is treated quickly, blindness can result. Unfortunately, two-thirds of those with closed-angle glaucoma develop it slowly without any symptoms prior to an attack. See a short video on Closed Angle Glaucoma.
Who is at risk for glaucoma?
Your ophthalmologist considers many kinds of information to determine your risk for developing the disease. The most important risk factors include:
- age
- elevated eye pressure
- family history of glaucoma
- African or Hispanic ancestry
- farsightedness or nearsightedness
- past eye injuries
- thinner central corneal thickness
- systemic health problems, including diabetes, migraine headaches, and poor circulation.
Your ophthalmologist will weigh all of these factors before deciding whether you need treatment for glaucoma, or whether you should be monitored closely as a glaucoma suspect. This means your risk of developing glaucoma is higher than normal, and you need to have regular examinations to detect the early signs of damage to the optic nerve.
How is glaucoma detected?
Regular eye examinations by your ophthalmologist are the best way to detect glaucoma. A glaucoma screening that checks only the pressure of the eye is not sufficient to determine if you have glaucoma. The only sure way to detect glaucoma is to have a complete eye examination.
Visual field testing is used to monitor the development of blind spots and peripheral or side vision.
During your glaucoma evaluation, your ophthalmologist will:

Visual field testing is used to monitor the development of blind spots and peripheral or side vision.
- measure your intraocular pressure (tonometry)
- inspect the drainage angle of your eye (gonioscopy)
- evaluate whether or not there is any optic nerve damage (ophthalmoscopy)
- test the peripheral vision of each eye (visual field testing, or perimetry).
Follow this link for more detailed information regarding the Visual Field Test for Glaucoma.
Photography of the optic nerve or other computerized imaging such as Optical Coherence Tomography may be recommended. Some of these tests may not be necessary for everyone. These tests may need to be repeated on a regular basis to monitor any changes in your condition.
Loss of vision can be prevented
Regular medical eye exams can help prevent unnecessary vision loss. Recommended intervals for eye exams are:
- Ages 20 to 29: Individuals of African descent or with a family history of glaucoma should have an eye examination every 3 to 5 years. Others should have an eye exam at least once during this period.
- Ages 30 to 39: Individuals of African descent or with a family history of glaucoma should have an eye examination every 2 to 4 years. Others should have an eye exam at least twice during this period.
- Ages 40 to 64: Every 2 to 4 years.
- Ages 65 or older: Every 1 to 2 years.
Glaucoma and how it is Detected
Glaucoma Implant Surgery
Mini-Filtration Implant
Trabecular Bypass Stent
Retinal Nerve Fibers and Glaucoma
Open Angle Glaucoma
Glaucoma and Blind Spots
Closed Angle Glaucoma
Laser Treatment for Glaucoma with ALT and SLT
Laser Trabeculoplasty
Laser Iridotomy
Trabeculectomy
Article Videos
- Anatomy of the Eye
- Botox
- Cataracts
- Diabetes and the Eye
- Diabetic Retinopathy – What is it and how is it detected?
- Treatment for Diabetic Retinopathy
- Non-Proliferative Diabetic Retinopathy (NPDR) – Video
- Proliferative Diabetic Retinopathy (PDR) – Video
- Cystoid Macular Edema
- Vitreous Hemorrhage – Bleeding from diabetes (Video)
- Vitrectomy Surgery for Vitreous Hemorrhage (Video)
- Macular Edema
- Laser Procedures for Macular Edema (Video)
- Laser for Proliferative Diabetic Retinopathy – PDR (Video)
- How the Eye Sees (Video)
- Dilating Eye Drops
- Dry Eyes and Tearing
- Eye Lid Problems
- A Word About Eyelid Problems
- Bells Palsy
- Blepharitis
- Blepharoptosis – Droopy Eyelids (Video)
- Dermatochalasis – excessive upper eyelid skin (Video)
- Ectropion – Sagging Lower Eyelids (Video)
- Entropion – Inward Turning Eyelids (Video)
- How to Apply Warm Compresses
- Ocular Rosacea
- Removing Eyelid Lesions
- Styes and Chalazion
- Twitches or Spasms
- Floaters and Flashes
- Glaucoma
- Selective Laser Trabeculoplasty (SLT) for Glaucoma
- Glaucoma: What is it and how is it detected?
- Optical Coherence Tomography OCT – Retina & Optic Nerve Scan
- Treatment for Glaucoma
- Retinal Nerve Fibers and Glaucoma (Video)
- Open Angle Glaucoma (Video)
- Closed Angle Glaucoma (Video)
- Visual Field Test for Glaucoma
- Glaucoma and Blind Spots (Video)
- Treatment for Glaucoma with Laser Iridotomy (Video)
- Laser Treatment for Glaucoma with ALT and SLT (Video)
- Surgical Treatment for Glaucoma with Trabeculectomy (Video)
- Surgical Treatment of Glaucoma with Seton (Video)
- Keeping Eyes Healthy
- Laser Vision Correction
- Latisse for Eyelashes
- Macular Degeneration
- Macular Degeneration – What is it and how is it detected?
- Treatment for Macular Degeneration
- Dry Macular Degeneration (Video)
- Wet Macular Degeneration (Video)
- Treatment of Macular Degeneration with Supplements
- Treatment of Wet Macular Degeneration with Anti-VEGF Injections
- Amsler Grid – A home test for Macular Degeneration (Video)
- Living with Vision Loss
- How the Eye Works – The Macula (Video)
- Other Eye Conditions
- Central Serous Retinopathy
- Lattice Degeneration of the Retina
- A Word About Other Eye Conditions
- Amblyopia
- Carotid Artery Disease and the Eye
- Fuch’s Corneal Dystrophy
- Herpes Simplex and the Eye
- Herpes Zoster (Shingles) and the Eye
- Ischemic Optic Neuropathy
- Keratoconus
- Macular Hole
- Macular Pucker
- Microvascular Cranial Nerve Palsy
- Migraine and the Eye
- Optic Neuritis
- Pseudotumor Cerebri
- Retinal Vein Occlusion
- Retinitis Pigmentosa
- Retinopathy of Prematurity
- Strabismus
- Thyroid Disorders and the Eye
- Uveitis
- Vitreomacular Adhesions / Vitreomacular Traction Syndrome
- Red Eye
- Refractive Errors
- Retinal Tears and Detachments
Disclaimer
This Patient Education Center is provided for informational and educational purposes only. It is NOT intended to provide, nor should you use it for, instruction on medical diagnosis or treatment, and it does not provide medical advice. The information contained in the Patient Education Center is compiled from a variety of sources. It does NOT cover all medical problems, eye diseases, eye conditions, ailments or treatments.
You should NOT rely on this information to determine a diagnosis or course of treatment. The information should NOT be used in place of an individual consultation, examination, visit or call with your physician or other qualified health care provider. You should never disregard the advice of your physician or other qualified health care provider because of any information you read on this site or any web sites you visit as a result of this site.
Promptly consult your physician or other qualified health provider if you have any health care questions or concerns and before you begin or alter any treatment plan. No doctor-patient relationship is established by your use of this site.